How Does Targeted Muscle Reinnervation (TMR) Aid in Prosthetic Control for Limb Loss Patients?
The evolution of medical science and technology has brought new hope and opportunities for individuals with limb loss. Amongst the innovative advancements in this field, Targeted Muscle Reinnervation (TMR) has emerged as a remarkable technique. It’s set to redefine the way patients interact with prosthetic limbs, paving the way for improved control and reduced pain. In this article, you will explore the intricacies of TMR, its role in prosthetic control, and its impact on patients.
Understanding Targeted Muscle Reinnervation (TMR)
Before delving into the specifics of how TMR aids in prosthetic control, it’s crucial to understand what this procedure entails. Targeted Muscle Reinnervation (TMR) is a surgical procedure developed to improve prosthetic control in patients who have undergone limb amputation.
Sujet a lire : What Is the Impact of Chewable Vitamin Supplements on Dental Health?
The primary purpose of TMR is to redirect nerves that once controlled the amputated limb towards residual muscles. When these nerves grow into the muscle, they can enable control of a myoelectric prosthesis. This process of nerve redirection and growth into a new muscle is the crux of TMR.
The Role of TMR in Prosthetic Control
The control of a prosthetic limb has always been a significant challenge for patients. Traditional prosthetic limbs rely on the muscles, skin, and nerves remaining after amputation to control the prosthesis. However, these methods are often limited in their ability to provide a natural and intuitive control. This is where TMR comes into play.
A lire également : What Strategies Enhance Language Development in Toddlers with Hearing Impairment?
TMR surgery allows the nerves that were previously responsible for limb movements to be connected to new, residual muscles. After the nerves have been reinnervated into the targeted muscles, they can respond to signals from the brain intended for the lost limb. These signals are then picked up by sensors in the prosthetic limb, allowing for more natural and intuitive control.
The Impact of TMR on Pain Management
Next to prosthetic control, pain management is a significant concern for patients who have undergone limb amputation. The phenomenon of ‘phantom limb pain’, where patients continue to feel pain or sensations from the amputated limb, is a common issue.
TMR can help in alleviating this pain. By re-routing the nerves that were severed during amputation into other muscles, the nerve signals which cause phantom limb pain can be reduced. Several studies available on PubMed and Google Scholar support the role of TMR in reducing residual and phantom limb pain, thus improving the overall quality of life for patients.
The Success Stories of TMR
TMR has shown promising results in numerous cases. Patients who have undergone TMR surgery have reported improved functionality of their prosthetic limbs, including better control of complex tasks such as grasping and lifting objects.
For instance, the case of a young woman who gained control of her prosthetic hand after undergoing TMR was documented in the Journal of Hand Surgery. After the surgery, she was able to perform tasks with her prosthetic hand that she had not been able to accomplish before, such as holding a cup, writing, and even typing. This case, among many others, illustrates the significant impact TMR can have on improving the quality of life for patients with limb loss.
The Future of TMR
While TMR has already proven to be a game-changer in the field of prosthetic limb control, ongoing research continues to enhance its potential. The future of TMR holds promising prospects in the realm of sensory feedback, where patients will not only be able to control but also feel their prosthetic limbs.
With the continuous advancements in technology and medical sciences, one can only imagine the potential TMR holds. It is hoped that these innovations will continue to improve the quality of life for those who have endured the loss of a limb, offering better control, functionality, and reduced pain.
Targeted Muscle Reinnervation (TMR) indeed represents a ray of hope for amputees worldwide. By enhancing prosthetic control and reducing pain, this revolutionary technique is helping patients regain control of their lives. As technology evolves and research progresses, the possibilities for further improvement seem limitless.
The Science Behind TMR: A Deeper Look
Targeted Muscle Reinnervation (TMR) is a fascinating procedure, grounded in complex neuroscience. While the technique may sound simple in explaining its use of nerve redirection to enhance prosthetic limb control, the process is in fact an intricate one that takes advantage of the human body’s innate adaptability.
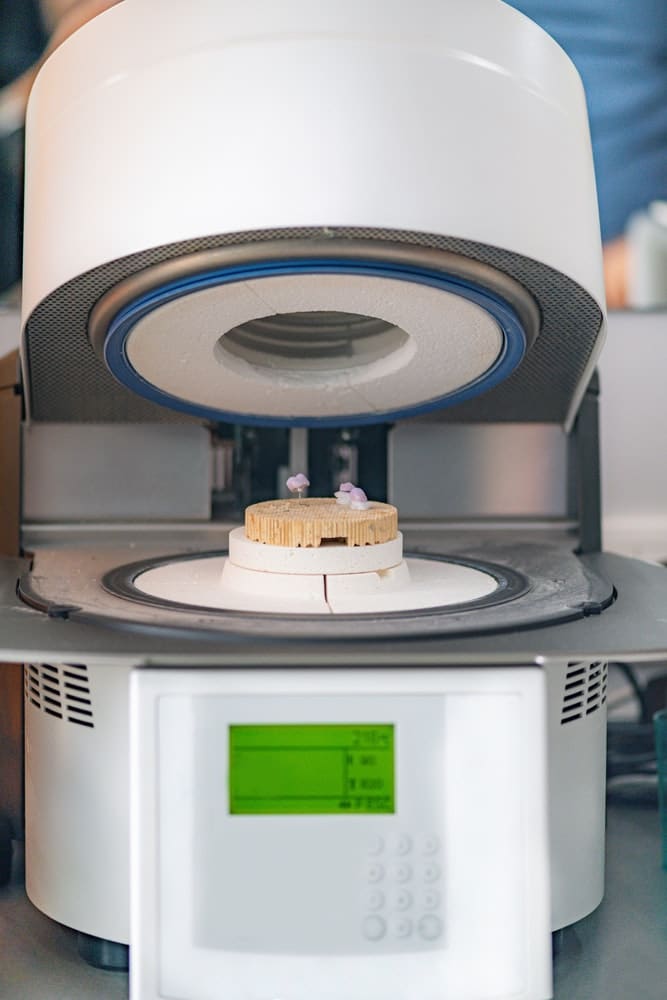
In TMR surgery, the residual limb’s nerves, which once controlled the amputated limb, are surgically redirected to control the remaining muscles. This redirection process is made possible because of the brain’s pattern recognition abilities. The brain continues to send signals intended for the missing limb, despite the limb’s absence. These signals are intercepted by the redirected nerves and result in muscular contractions, which are then detected by sensors within the prosthetic limb.
These sensors, often myoelectric in nature, are designed to pick up the EMG signals from muscular contractions. The sensors then translate these signals into commands that control the prosthetic limb’s movements. As a result, patients can control their prostheses intuitively, just by thinking about the movement they want to make. This significant leap in prosthetic technology was made possible by our growing understanding of the brain’s plasticity and adaptability.
The Challenges and Limitations of TMR
While TMR is a groundbreaking technique, it’s important to acknowledge that, like any medical procedure, it doesn’t come without challenges and limitations. For one, the procedure requires a high level of surgical precision, as the redirection of nerves to target muscles must be done carefully, without causing additional damage to the soft tissue.
Potential complications can also emerge post-surgery. Neuroma pain, caused by nerve tissue growth, can develop at the surgery site. Additionally, not all patients are suitable candidates for TMR. The procedure is generally more effective for upper limb amputees, as lower limb amputations may not have sufficient residual nerves to redirect.
However, despite these limitations, the benefits of TMR far outweigh the challenges. With the continuous improvement in surgical techniques and prosthetic technology, these limitations are gradually being overcome.
Conclusion: The Power of TMR Surgery
In conclusion, Targeted Muscle Reinnervation (TMR) is revolutionizing the field of prosthetic limb control. By tapping into the body’s natural pattern recognition abilities and the brain’s adaptability, TMR allows patients to control their prosthetic limbs in a more natural and intuitive manner.
This technique is not just about improving physical functionality; it’s about restoring a sense of normalcy and improving the overall quality of life for individuals who have endured limb loss. From providing relief from phantom limb pain to enabling a higher level of independence, TMR is a testament to the immense potential of medical science.
Research papers available on platforms such as PubMed and Google Scholar highlight the efficacy of TMR in improving prosthetic functionality and pain management.
Looking towards the future, we can expect to see even more advancements in this field. The possibilities of sensory feedback and further improvement in prosthetic control are already on the horizon. By continuously expanding our understanding and harnessing the potential of TMR, we are opening up a world of possibilities for individuals with limb loss.
